Fascia and "kanshoho"
Explanatory Video
Relationship between Fascia and "kanshoho"
In 2018, the International Classification of Diseases underwent its first major revision in 30 years, resulting in the 11th edition (ICD-11). In ICD-11, Fascia has been incorporated as a fundamental component of body composition, garnering international attention for the concept of Fascia.
According to Bruno Bordoni and colleagues in the United States (1),
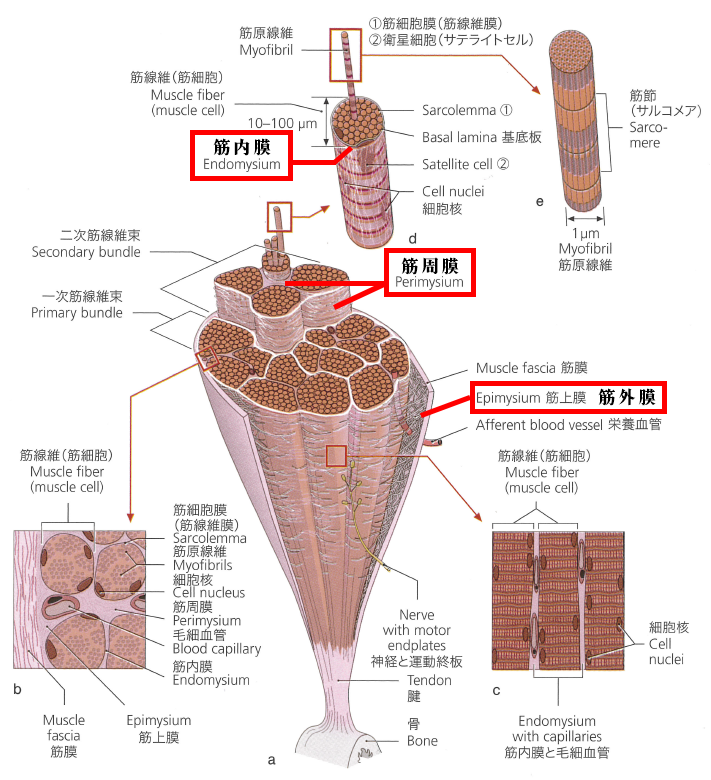
Fascia is a tissue that includes the capacity to respond to mechanical stimulation. It encompasses various tissues, both liquid and solid, including the epidermis, dermis, fat, blood, lymph, blood vessels and lymphatic vessels, nerve filaments covering tissues (endoneurium, perineurium, epineurium), voluntary striated muscle fibers and the tissues that surround and penetrate them (epimysium, perimysium, endomysium), ligaments, tendons, tendon sheaths, cartilage, bone, meninges, involuntary smooth muscle tissues (all derived from the mesoderm), visceral ligaments, skin (both small and large), peritoneum, and the tongue.
This continuous network of tissue is constantly transmitting and receiving mechanical and metabolic information that may potentially influence the shape and function of the entire body.
Because Fascia is a tissue in the interstitium that is constantly transmitting and receiving mechanical and metabolic information, it includes gel-like tissues such as collagen-based fascia, colloids, reticulin, fibronectin, and others.
Before the development of “kanshoho”, it was understood that the stiffness of muscles was related to the “interstitium (fascia).” In 2007, the treatment method “kanshoho” was developed to solubilize the gel formation in the “interstitium (fascia).”
In Japan, the Japan Society of Orthopedic Internal Medicine Research Association, a nonprofit organization, was established in 2018. They have provided the following definitions for “Fascia” in both medical and general terms:

(Medical Terminology) “A fascia” = A visible fibrous structure with network functions (April 2019, JNOS).
Here, “network functions” refer to the system that connects and supports various tissues and organs and perceives them.
In English, it is expressed as “macroscopic anatomical structures forming of fibrils with the function of fascial network system.”
This definition corresponds to “A facsia” in English (macroscopic anatomical term).
The term “fascia” (General Terminology) = A three-dimensional fibrous network structure that covers, connects, and transmits information throughout the body. It smoothes the movement of organs, supports and protects them, and maintains their position (March 2020, JNOS).
For media and patient information, it is recommended to use this definition.
Related term: For reference, “Myofascia” is defined as follows:
(General Terminology) Fibrous tissue that wraps individual muscle fibers, muscles, or muscle groups, dividing and connecting them. It smoothes the movement of muscles and joints while controlling their position (March 2020, JNOS).
In other words, “Myofascia” is a part of “fascia.”
According to the definition by Bruno Bordoni and colleagues in the United States (1), the definition provided by the Japan Society of Orthopedic and Internal Medicine Research is narrower, referring to “fibrous tissues including myofascia.” However, in this text, in accordance with international standards, it broadens the definition to include colloids (colloidal tissues) that are closely related to muscle stiffness and muscle tension. Hence, it encompasses “interstitium (Fascia)” in a more general sense.
In recent years, there has been an increase in treatment methods referred to as “hydro release” (*1) and “myofascial release” (*2).
The hydro release and myofascial release techniques conducted by the Japan Society of Orthopedic and Internal Medicine Research aim to improve movement by targeting the fascia, specifically the myofascia, which is a part of it. These techniques are believed to have an impact on the muscular fascia as well.
(Source: “Prometheus Atlas of Anatomy, 2nd Edition, 2013,” p. 56, modified)
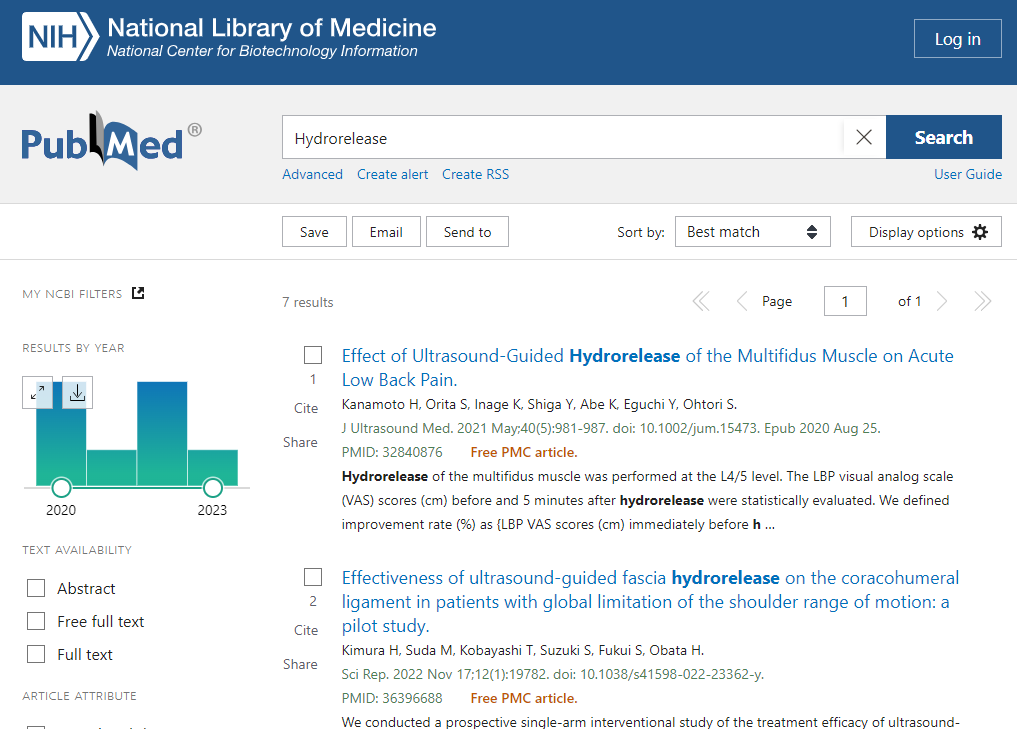
As of August 2023, when searching for “Hydrorelease” on PubMed, there are 7 results, all of which are contributed from Japan. This indicates that Hydrorelease is a new treatment concept originating from Japan.
While it’s understood that Hydrorelease, performed under ultrasound guidance, offers high reproducibility, it’s important to note that Hydrorelease involves the injection of liquids such as physiological saline, low-concentration anesthetics, and hyaluronic acid into the fascia, which is part of the interstitium. This injection process is invasive and cannot deny the occurrence of events or risks that disrupt homeostasis within the body.
Additionally, in hydro release and fascial release, because the approach is to the epimysium, a slight part of the interstitium (fascia), the effect reaches up to the perimysium, resulting in temporary muscle relaxation.
With this approach, it is challenging to effectively relax the muscles and sustain that relaxation. Even if only certain parts of the epimysium and perimysium allow for improved sliding, if the widespread, overall sliding of the epimysium, perimysium, and endomysium is not enhanced, the muscles won’t function normally, and muscle stiffness will persist. Moreover, muscle stiffness is likely to return quickly.
This results in a situation where the patient’s symptoms may temporarily improve on the spot but are prone to recurrence, a phenomenon known as “remission recurrence,” which does not lead to a lasting cure for the patient.
From an anatomical perspective, if a muscle is composed of six compartments with a diameter of 3 cm, the area of the epimysium is approximately 1/30,000 when compared to the combined area of the perimysium and endomysium. Furthermore, the combined area of the epimysium and perimysium is approximately 1/870 when compared to the area of the endomysium. This helps to understand that hydro release or fascial release techniques are approaches targeting only an extremely small part of the “interstitium (fascia),” whereas “kanshoho” has an effect on the “interstitium (fascia)” that is at least 870 times greater.
I won’t specifically cite the source, but if you perform a web search for “Hydrorelease effectiveness duration,” you can find practical information from clinical practitioners who use Hydrorelease. Some mention immediate pain relief, stating that the pain at the injection site can be relieved for about an hour, or that the duration of effectiveness can vary from overnight to several days or even a week, with no fixed injection interval. Some recommend getting the injections on consecutive days or 2-3 times a week, especially when experiencing strong pain or stiffness.
However, the “interstitium (Fascia)” is not limited to just the epimysium that hydro release and fascial release target.
Within the “interstitium (Fascia),” there is epimysium that surrounds the entire muscle, perimysium that encases muscle bundles, and endomysium that envelops muscle fibers.
“kanshoho“ approaches the interstitium (fascia), including the epimysium, perimysium, and endomysium, and by transforming the gel state of the fascia into a sol state, it achieves a state of near-complete muscle relaxation.
“kanshoho” is also characterized by its ability to transform the gel state of the interstitium (fascia) into a sol state, allowing not only the muscles but also the subcutaneous tissue (subcutaneous fat) that has hardened to be brought into a state of near-complete.
However, the “interstitium (Fascia)” is not limited to just the epimysium that hydro release and fascial release target.
Within the “interstitium (Fascia),” there is epimysium that surrounds the entire muscle, perimysium that encases muscle bundles, and endomysium that envelops muscle fibers.
“kanshoho“ approaches the interstitium (fascia), including the epimysium, perimysium, and endomysium, and by transforming the gel state of the fascia into a sol state, it achieves a state of near-complete muscle relaxation.
“kanshoho” is also characterized by its ability to transform the gel state of the interstitium (fascia) into a sol state, allowing not only the muscles but also the subcutaneous tissue (subcutaneous fat) that has hardened to be brought into a state of near-complete.
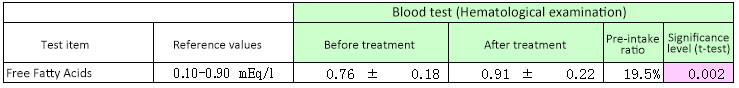
Furthermore, “kanshoho” has been found to increase free fatty acids in venous blood even after a 10-minute treatment, indicating enhanced lipid breakdown from metabolites.
“kanshoho” has evolved from basic research into a scientifically supported therapy that can improve pain and discomfort and promote overall health.
We strongly encourage the adoption of “kanshoho” in the medical field to help alleviate the suffering of patients dealing with pain and illness, and to collectively save as many individuals as possible.
(*1) Hydrorelease is the act of injecting liquids such as saline solution, low-concentration anesthetics, hyaluronic acid, and others into the fascia, which is part of the interstitium.
(*2) Fascial release is the act of improving the sliding properties of the epimysium, which is part of the interstitium.
(1) Bordoni B, Mahabadi N, Varacallo M. Anatomy, Fascia. 2023 Jul 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–.